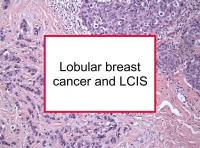
Approximately 10% to 12% of U.S. invasive breast cancers are classified as lobular, which refers to the fact that the cancer developed in the cells that line the milk-producing glands (lobules) of the breast. The most common histological type of breast cancer, accounting for approximately 70% of cases, is ductal breast cancer, which forms in the milk ducts.
Almost half of women diagnosed with lobular breast cancer are treated with mastectomy, either initially or after a lumpectomy that does not result in clean margins.
Lobular breast cancer is more likely to be multifocal (more than one tumor per breast), bilateral (diagnosed in both breasts at the same time), and both estrogen receptor positive and progesterone receptor positive (ER+/PR+) than ductal breast cancer. It is rare for lobular disease to be HER2 positive. Lobular breast cancer is more prone to late recurrence. Women diagnosed with LCIS concurrently with invasive breast cancer at initial surgery appear to be at higher risk for subsequent contralateral breast cancer than those without LCIS.
Lobular breast cancer is more likely to have a hereditary component. In fact, lobular breast cancer patients are more likely than other breast cancer patients to have a father diagnosed with cancer, especially prostate cancer.
Use of hormone replacement therapy (HRT), including estrogen-only hormone therapy, has been shown to increase the risk of lobular breast cancer, as has use of levonorgestrel intrauterine system (LNG-IUS), an IUD-type device. Long-term statin use was also found to be associated with increased risk of lobular breast cancer in one study.
Some researchers have suggested that chemotherapy is not useful or even contraindicated for lobular breast cancer. However, this is unproven. One study reported that treatment with the aromatase inhibitor letrozole (Femara) resulted in better disease-free survival than tamoxifen in women with ER+ lobular breast cancer. In any event, it makes sense that treatment decisions should be based on factors such as tumor size, lymph node status, proliferation index (Ki-67), hormone receptor status, and other prognostic factors in addition to the histological type.
Women with lobular breast cancer are more likely to get ovarian and gastric (stomach) metastases than those with other types of breast cancer.
LCIS
Women with lobular carcinoma in situ (LCIS) or atypical lobular hyperplasia (a possible precursor of both LCIS and invasive breast cancer) are at significantly higher than average risk for invasive breast cancer, but the risk is higher for developing both ductal and lobular breast cancer. LCIS is found in fewer than 2% of all breast cancers. Lobular neoplasia is a global term that refers to both LCIS and atypical lobular hyperplasia.
One small study reported that 50% of invasive lobular tumors eventually arising in women with LCIS were clonally related, in other words, they were very similar genetically with shared mutations. A total of 58% of ductal carcinoma in situ (DCIS) lesions developing in women with LCIS were clonally related, but with a lower number of shared mutations than that found in LCIS to lobular cases. No evidence of a clonal relationship was found in any of the cases of invasive ductal breast cancer arising in women with LCIS.
A 2023 study reported that the absence of LCIS at the time of diagnosis was an unfavorable prognostic marker among with those invasive lobular breast cancer. Pure invasive lobular breast cancer was more likely to be associated with higher stages at diagnosis compared to lobular breast cancer plus LCIS.
LCIS has familial component
First degree (parent, sibling or child) and second degree (grandparent, aunt/uncle, half-sibling) relatives of women with LCIS have a higher risk of invasive breast cancer than the general population, as one large 2020 Swedish prospective study reported. In fact, the authors found that the 10-year cumulative risk of a 50-year old woman with a first or second degree relative with LCIS was similar to the risk of one with such a relative with invasive breast cancer.
Risk of progression from LCIS to invasive breast cancer
One 2024 study reported that LCIS has both an immediate risk (19.3%) and a delayed risk (18.6%) of invasive breast cancer with 91% of such cancer occurring in the same breast as the LCIS and 9% in the opposite (contralateral) breast.
A 2020 study found that 7.8% of women with atypical hyperplasia and 5.7% of women with LCIS developed invasive breast cancer during the first ten years after diagnosis. Another study reported that the seven-year cumulative invasive breast cancer incidence was 9.9% after an initial diagnosis of atypical hyperplasia or LCIS.
However, the cumulative risk of developing invasive breast cancer appears to continue to grow over time. A Canadian study reported that the 20-year cumulative risk of developing invasive breast cancer was 21.3% for LCIS patients. Another study reported that the annual incidence of breast cancer (including DCIS) was 2% among women with LCIS.
Another study concluded that women under age 35 diagnosed with LCIS and other forms of atypical hyperplasia should be followed closely, receiving annual breast cancer screening starting at age 25 or age of diagnosis. This was based on the fact that 12% of such women developed breast cancer within a median of 90 months.
Efforts to predict which LCIS patients will progress to invasive breast cancer have not been very successful. However, one study found that LCIS with high Ki-67 (a marker of proliferation) expression is more likely to progress to invasive breast cancer than low Ki-67. Women with high breast density are also more likely to progress, as are women using HRT. In addition, LCIS that can be detected manually (palpable LCIS) is more likely to progress to invasive breast cancer. Note that palpable LCIS may feel like an area of thickening or firmness rather than a lump.
Since the majority of women with LCIS do not go on to develop invasive breast cancer, some do not undergo surgery to remove the LCIS lesion. Rather, they are placed under increased surveillance and they may receive endocrine treatment. However, since a substantial minority of women diagnosed with LCIS based on core needle biopsy are found to have invasive breast cancer upon open surgical biopsy, some experts are of the opinion that surgical excision should follow needle biopsy to confirm that the diagnosis is limited to noninvasive breast cancer. It is also important for women who do progress to invasive breast cancer to have all of their LCIS surgically removed.
The picture is more clear for pleomorphic lobular carcinoma in situ (PLCIS), a higher-risk type of LCIS which is more likely to progress. When patients are diagnosed with PLCIS using a needle biopsy, the lesion should be surgically removed. In addition, re-excision should be performed if any PLCIS or LCIS is found at or near the surgical margins.
Diagnosing lobular breast cancer
Lobular breast cancer is less visible on mammograms, sonograms and breast MRIs than ductal breast cancer because the cancer cells infiltrate between normal cells in a very regular manner. Typically, lobular breast cancer does not form a discrete lump. Instead, the breast may feel thicker or more firm in the area of the tumor. Because of these factors, lobular breast cancer often is diagnosed when it has reached a larger diameter than other types of breast cancer. Some researchers have recommended that an MRI of both breasts be performed when lobular breast cancer is diagnosed based on a biopsy in order to find other tumors that might be present. Use of MRIs has also been recommended for follow up after treatment.
Despite the difficulty in imaging lobular breast cancer, since this type typically does not behave aggressively, lobular breast cancer patients tend to have a relatively good prognosis. On the other hand, lobular breast cancer that is palpable (i.e., can be detected manually) is associated with higher tumor grade and poorer survival than lobular cancer that cannot be felt by hand. Also, lobular breast cancer can relapse many years after initial diagnosis and treatment.
Please see our article on diet for lobular breast cancer patients and survivors information pertaining to diet and supplements. We suggest that LCIS and lobular breast cancer patients and survivors also refer to the articles that discuss their individual breast cancer subtypes (e.g., ER+/PR+, ER+/PR-, triple negative).
Below are links to 20 recent studies concerning this topic. For a more complete list of studies, and more articles concerning lobular breast cancer and LCIS, please click on the tags lobular breast cancer or LCIS.